Decoding HRT: Everything You Need to Know About Hormones and Therapy

Understanding Hormones and Their Role in Your Health Journey
Hormones and HRT (Hormone Replacement Therapy) are a critical area of healthcare, especially for women navigating menopause and others with hormonal imbalances. Here's what you need to know:
Key Facts About Hormones and HRT:
- HRT Definition: Replaces hormones (estrogen, progesterone, testosterone) that decline during menopause.
- Primary Use: Treats moderate-to-severe menopausal symptoms like hot flashes, night sweats, and vaginal dryness.
- Types: Systemic HRT (affects the whole body) and local HRT (targets specific areas).
- Administration: Pills, patches, gels, sprays, rings, and pellets.
- Timing Matters: Most beneficial when started before age 60 or within 10 years of menopause.
- Modern Options: Bio-identical hormones derived from natural sources offer safer alternatives.
The landscape of hormone therapy has changed dramatically. Modern bio-identical HRT is often safer and more effective than older synthetic versions. Research shows that 74% of postmenopausal women younger than 55 experience vasomotor symptoms, with 28% reporting moderate or severe symptoms that significantly impact quality of life.
For many, HRT is about reclaiming vitality, improving bone health, and reducing long-term health risks.
I'm Dr. Gannon Ward. In my years of holistic wellness practice, I've seen how hormones and HRT can transform lives. Combining hormone therapy with complementary treatments, like those at Atmosphere Chiropractic & Wellness, creates the most effective outcomes for long-term wellness.
Important hormones and hrt terms:
What is Hormone Replacement Therapy (HRT) and Why is it Used?
Hormone Replacement Therapy (HRT) is a medical treatment that replenishes hormones your body produces less of as you age, helping your body run smoothly again. While widely known for helping women through menopause, it addresses any significant hormonal decline affecting your quality of life.
The menopausal transition is a natural journey, typically between ages 45 and 55, that unfolds in stages:
- Perimenopause: The transition phase, lasting several years, where hormone levels fluctuate and periods become irregular.
- Menopause: Confirmed after 12 consecutive months without a period, marking a significant drop in estrogen production.
- Postmenopause: Includes all the years after menopause. Effective treatment is crucial as many women spend a third of their lives in this stage.
During these stages, the ovaries reduce the production of estrogen, progesterone, and some testosterone. This hormonal decline triggers uncomfortable symptoms. HRT steps in to replace these missing hormones, alleviating symptoms and restoring well-being.
For more detailed information about how this therapy works, you can explore more info about Hormone Replacement Therapy.
The Main Symptoms HRT Can Treat
Menopausal symptoms can be life-disrupting, but hormones and HRT can provide significant relief. Key symptoms include:
- Vasomotor Symptoms: This category includes hot flashes (sudden, intense feelings of heat) and night sweats (hot flashes during sleep), which disrupt daily life and rest.
- Genitourinary Syndrome of Menopause (GSM): This refers to changes in the vaginal and urinary tracts. Vaginal atrophy (thinning tissues) leads to dryness and painful intercourse, affecting intimacy and comfort.
- Mood Swings: Hormonal shifts can cause irritability, anxiety, and feelings of sadness.
- Sleep Disturbances: Beyond night sweats, hormonal changes can make it difficult to fall or stay asleep.
- Brain Fog: Many women experience frustrating memory lapses and difficulty concentrating.
- Reduced Libido: A combination of physical discomfort and hormonal changes can lower sexual desire.
HRT offers a path back to feeling more like yourself by addressing these symptoms directly.
The Hormones Involved in Therapy
Understanding the key hormones in HRT helps in making informed decisions:
- Estrogen: The primary hormone that declines during menopause. It regulates the reproductive system, maintains bone density, and keeps vaginal tissues healthy. Its decline has widespread effects.
- Progesterone: Crucial for women with a uterus. Progesterone (or its synthetic form, progestin) provides endometrial protection by preventing the uterine lining from thickening when taking estrogen, which reduces cancer risk.
- Testosterone: This hormone also declines with age. While not FDA-approved for female menopause symptoms, some women benefit from small amounts for energy, mood, and libido, prescribed by experienced providers.
The combination of hormones used in HRT is highly individualized based on your symptoms, medical history, and whether you've had a hysterectomy.
For more comprehensive information about how these hormones work specifically for women, check out Hormone Therapy for Women.
The Comprehensive Guide to Hormones and HRT Treatments
Finding the right hormones and HRT treatment requires individualized medical consultation. Every woman's body is different, and the best approach is one custom to your specific needs.

| Type of HRT | Targeted Symptoms | Forms | Systemic Absorption |
|---|---|---|---|
| Systemic HRT | Hot flashes, night sweats, mood swings, bone loss, widespread menopausal symptoms | Oral pills, skin patches, gels, sprays, subcutaneous pellets | Absorbed into the bloodstream, affects the entire body |
| Local HRT | Vaginal dryness, painful intercourse, urinary symptoms (Genitourinary Syndrome of Menopause) | Vaginal creams, tablets, rings | Primarily affects the local tissue, minimal systemic absorption |
Understanding the different types of hormones and HRT
HRT can be a full-body approach or provide targeted relief.
- Systemic HRT delivers hormones throughout the body via the bloodstream. It's ideal for widespread symptoms like hot flashes, night sweats, mood swings, and bone loss.
- Local HRT delivers low-dose estrogen directly to vaginal tissue via creams, tablets, or rings. It's a great option for women who only need relief from vaginal dryness and urinary symptoms, as it has minimal systemic absorption and fewer risks.
Your medical history determines the specific type of therapy:
- Estrogen-only therapy is for women who have had a hysterectomy (uterus removal). Without a uterus, progesterone is not needed.
- Combined Estrogen-Progestin Therapy (EPT) is for women who still have their uterus. The progestin provides uterus protection by preventing the uterine lining from overgrowth, which reduces cancer risk.
How HRT is Administered
Modern hormones and HRT come in various delivery methods to fit your lifestyle:
- Oral pills: Convenient daily pills, but they are processed by the liver, which may slightly increase blood clot risk.
- Transdermal patches: Applied to the skin once or twice a week. They bypass the liver, carrying a lower blood clot risk than oral pills.
- Gels and sprays: Applied daily to the skin, also bypassing the liver.
- Vaginal rings, creams, and tablets: Provide targeted, local relief for vaginal symptoms with minimal whole-body effects. Rings are replaced every three months, while creams and tablets are used a few times per week.
- Subcutaneous Hormone Pellets: Tiny implants placed under the skin that provide steady hormone levels for several months, offering maximum convenience.
Common HRT Treatment Routines
Your treatment routine depends on your menopausal stage:
- Sequential HRT (or cyclical therapy) is for women in perimenopause. It involves daily estrogen with progestogen for 10-14 days a month, which mimics a natural cycle and causes a predictable monthly bleed.
- Continuous combined HRT is for postmenopausal women (no period for at least a year). It involves taking both estrogen and progestogen daily, which usually stops vaginal bleeding after an adjustment period.
The right routine for you will be determined in consultation with your provider based on your health and preferences.
Weighing the Evidence: The Benefits and Risks of HRT
The conversation around hormones and HRT has been confusing, largely due to initial interpretations of the Women's Health Initiative (WHI) trial from the 1990s. Initial WHI results suggested increased risks of breast cancer, heart disease, and stroke, which scared many women away from HRT.
However, further analysis revealed the "timing hypothesis": the risks were higher for older women (average age 63) who started HRT more than 10 years after menopause. When you start HRT matters. Today, we know that for healthy women starting HRT before age 60 or within 10 years of menopause, the benefits usually outweigh the risks. The duration of use also plays a role, making individualized assessment crucial. For the most current medical consensus, you can review The 2022 Hormone Therapy Position Statement of The North American Menopause Society.
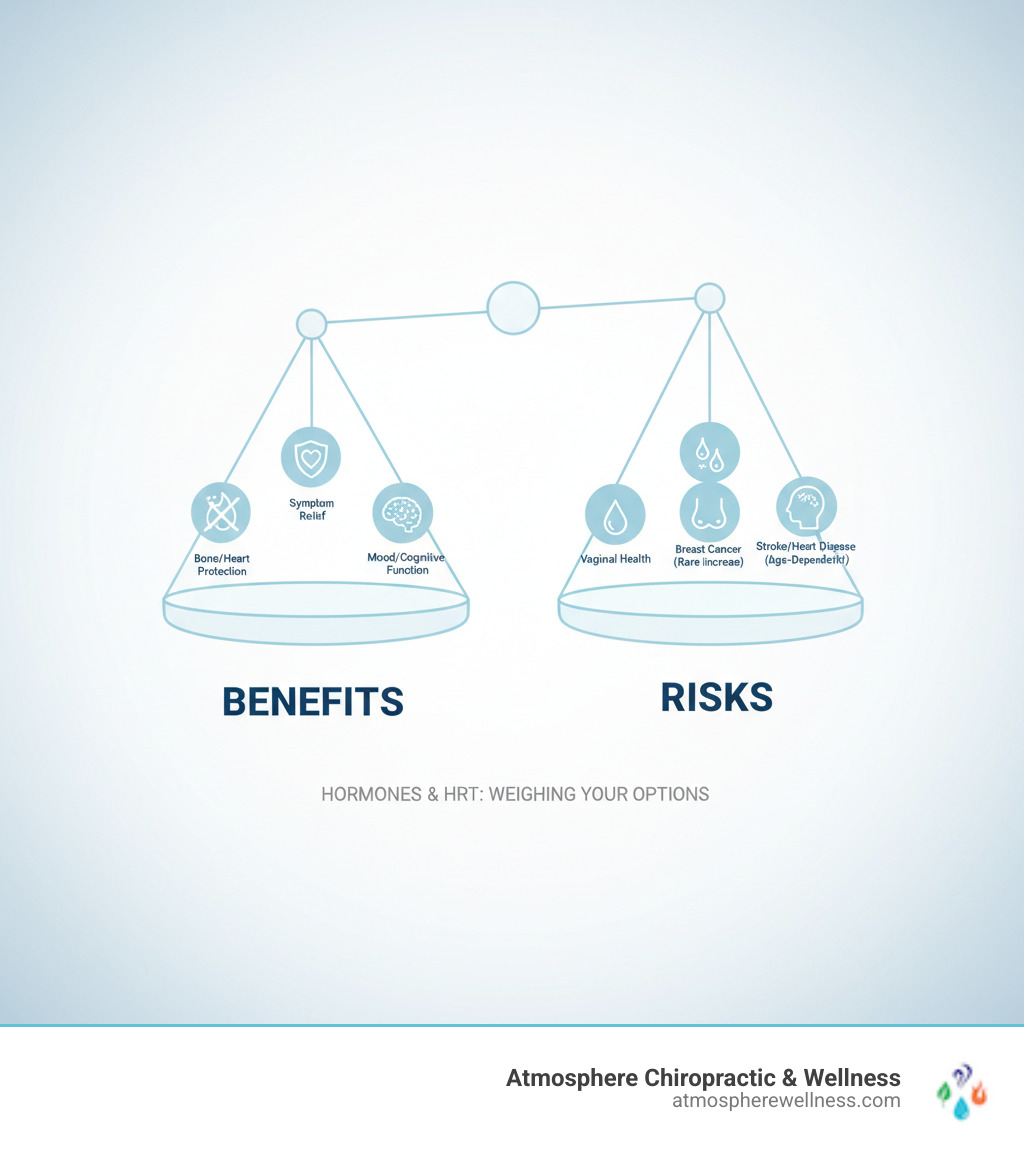
The Potential Benefits of Taking HRT
When used appropriately, the benefits of hormones and HRT can be life-changing:
- Symptom Relief: HRT effectively treats hot flashes, night sweats, and vaginal dryness, dramatically improving daily comfort and sleep.
- Bone Health: HRT is FDA-approved to prevent osteoporosis by slowing bone loss that accelerates after menopause, significantly reducing fracture risk.
- Mood and Cognitive Function: Many women report improved mental clarity, mood stability, and reduced "brain fog" with HRT.
- Cardiovascular Health: For women starting HRT before age 60, it may reduce heart disease risk by positively affecting cholesterol and blood vessels.
- Other Benefits: Some studies suggest a reduced risk of colorectal cancer. HRT also helps maintain skin moisture and elasticity.
Potential Risks and Side Effects
It's important to discuss potential risks, which are generally small for healthy women who start HRT at the right time.
- Blood Clots: Oral estrogen carries a small increased risk. Transdermal forms (patches, gels) largely avoid this risk as they bypass the liver.
- Stroke: Risk is slightly increased, particularly with oral HRT in older women.
- Heart Disease: Risk may increase if HRT is started more than 10 years after menopause, but may decrease for those who start earlier.
- Breast Cancer: Long-term use (5 or more years) of combined HRT (estrogen plus progestin) may slightly increase risk. Estrogen-only HRT has shown a neutral or slightly reduced risk.
- Ovarian and Uterine Cancer: Long-term combined HRT may slightly increase ovarian cancer risk. Uterine cancer risk increases if estrogen is taken without progestin in women with a uterus.
- Gallbladder Disease: Risk may increase, especially with oral estrogen.
Common side effects like breast tenderness, bloating, or headaches are usually mild and temporary, often resolving as the body adjusts. If side effects are bothersome, your treatment can often be adjusted. For more details, explore Bioidentical Hormone Replacement Therapy Pellets Side Effects.
Making an Informed Decision: Candidacy, Alternatives, and Modern Perspectives
Deciding on hormones and HRT is a process of shared decision-making between you and your provider. It involves a thorough risk assessment and a review of your symptoms, health history, and personal preferences to create the best plan for you.
At Atmosphere Chiropractic & Wellness, we partner with you to ensure you feel confident about your choices.
Who is a Good Candidate for HRT (and Who Should Avoid It)?
Many women are excellent candidates for HRT. Good candidates typically are:
- Healthy women under 60 (or within 10 years of menopause) with moderate to severe symptoms.
- Women needing osteoporosis prevention.
- Women with Premature Ovarian Insufficiency (POI), for whom HRT is essential for long-term health.
However, HRT is generally avoided by those with a personal history of:
- Hormone-sensitive cancers (e.g., breast, uterine).
- Blood clots, stroke, or heart attack.
- Unexplained vaginal bleeding.
- Active liver disease.
These are general guidelines; your individual situation requires a personal consultation.
Are Bioidentical Hormones a Safer Option?
Bioidentical hormones are chemically identical to human hormones, often derived from plants. It's important to distinguish between two types:
- FDA-approved bioidentical hormones (e.g., micronized progesterone, estradiol) are proven safe and effective through rigorous testing.
- Compounded bioidentical hormones are custom-mixed by pharmacies but are not FDA-regulated, meaning their long-term safety and efficacy are not well-established. The ACOG clinical consensus on compounded bioidentical hormones advises caution.
Our approach focuses on scientifically-backed treatments that are safe and effective.
The role of lifestyle factors with hormones and HRT
Hormones and HRT work best as part of a holistic wellness plan. Key lifestyle factors include:
- Diet: A whole-foods diet supports hormone processing and can reduce symptom severity.
- Exercise: Regular cardio and strength training improves mood, sleep, bone health, and can reduce hot flashes.
- Weight Management: Maintaining a healthy weight can lessen symptom severity.
- Stress Reduction: Managing stress through yoga, meditation, or other practices is crucial for hormonal balance.
- Smoking and Alcohol: Quitting smoking and limiting alcohol is vital, as both worsen symptoms and increase HRT-related risks.
Supportive Approaches to Hormonal Wellness
At Atmosphere Chiropractic & Wellness, we believe true wellness comes from an integrated approach. We combine hormones and HRT with complementary therapies to support your body's natural healing.
- Chiropractic Care: Proper spinal alignment supports the nervous system, which can positively influence your endocrine (hormone) system.
- Cryotherapy: Reduces inflammation, boosts mood, and improves sleep and energy.
- Red Light Therapy: Stimulates cellular repair to reduce inflammation, improve skin health, and boost vitality.
- Massage Therapy: Reduces stress, improves sleep, and relieves muscle tension.
Having these therapies under one roof in Lehi, Utah, allows for a unique, comprehensive approach. Combining HRT with these supportive treatments creates a synergistic effect for the best possible outcome.
Frequently Asked Questions about Hormones and HRT
Here are answers to some of the most common questions we hear from patients considering hormones and HRT.
How long is HRT typically taken and when should it be stopped?
There is no mandatory "stop date" for HRT; treatment duration is individualized. The goal is to use it for the shortest effective duration needed for symptom relief. An ongoing conversation with your provider is key to re-evaluate your needs annually. When stopping, a gradual taper is often recommended to minimize the return of symptoms.
Can HRT cause weight gain?
Scientific evidence shows that HRT itself does not cause weight gain. Instead, the metabolic changes of menopause often lead to weight gain, particularly around the midsection. By balancing hormones, HRT can help manage weight. Initial side effects like mild bloating or water retention are usually temporary.
Can I take HRT if I have a history of cancer?
This is a complex question requiring a highly individualized answer in consultation with your oncologist.
- For breast cancer survivors (especially hormone-sensitive types), systemic HRT is generally not recommended. However, local vaginal estrogen for severe symptoms may be an option.
- Women with a history of uterine cancer are also generally advised against HRT.
- For a history of other cancers, HRT may be possible, but each case requires careful evaluation by your full medical team.
Any decision about HRT after a cancer diagnosis requires a detailed discussion between you, your oncologist, and your HRT provider. For more, see research on Managing menopause after cancer.
Conclusion
Navigating hormones and HRT is about reclaiming control over your health during a natural life transition. For most healthy women who start modern HRT before age 60 or within 10 years of menopause, the benefits often significantly outweigh the risks.
Your health journey is unique. The decision to use hormones and HRT is an ongoing partnership with your healthcare provider, custom to your specific needs. It's not a one-time decision, but an evolving conversation focused on your goals.
At Atmosphere Chiropractic & Wellness in Lehi, Utah, we believe in a multi-angled approach to wellness. We know that combining HRT with our other innovative therapies--chiropractic care, cryotherapy, red light therapy, and massage--creates a powerful synergistic effect. This comprehensive approach helps you build a foundation for long-term vitality, not just manage symptoms.
If you're ready to see how balanced hormones and HRT, supported by our integrated wellness services, can help you reclaim your energy and confidence, we're here to help. Start your personalized HRT journey with us to experience comprehensive care.

Understanding Hormones and Their Role in Your Health Journey
Hormones and HRT (Hormone Replacement Therapy) are a critical area of healthcare, especially for women navigating menopause and others with hormonal imbalances. Here's what you need to know:
Key Facts About Hormones and HRT:
- HRT Definition: Replaces hormones (estrogen, progesterone, testosterone) that decline during menopause.
- Primary Use: Treats moderate-to-severe menopausal symptoms like hot flashes, night sweats, and vaginal dryness.
- Types: Systemic HRT (affects the whole body) and local HRT (targets specific areas).
- Administration: Pills, patches, gels, sprays, rings, and pellets.
- Timing Matters: Most beneficial when started before age 60 or within 10 years of menopause.
- Modern Options: Bio-identical hormones derived from natural sources offer safer alternatives.
The landscape of hormone therapy has changed dramatically. Modern bio-identical HRT is often safer and more effective than older synthetic versions. Research shows that 74% of postmenopausal women younger than 55 experience vasomotor symptoms, with 28% reporting moderate or severe symptoms that significantly impact quality of life.
For many, HRT is about reclaiming vitality, improving bone health, and reducing long-term health risks.
I'm Dr. Gannon Ward. In my years of holistic wellness practice, I've seen how hormones and HRT can transform lives. Combining hormone therapy with complementary treatments, like those at Atmosphere Chiropractic & Wellness, creates the most effective outcomes for long-term wellness.
Important hormones and hrt terms:
What is Hormone Replacement Therapy (HRT) and Why is it Used?
Hormone Replacement Therapy (HRT) is a medical treatment that replenishes hormones your body produces less of as you age, helping your body run smoothly again. While widely known for helping women through menopause, it addresses any significant hormonal decline affecting your quality of life.
The menopausal transition is a natural journey, typically between ages 45 and 55, that unfolds in stages:
- Perimenopause: The transition phase, lasting several years, where hormone levels fluctuate and periods become irregular.
- Menopause: Confirmed after 12 consecutive months without a period, marking a significant drop in estrogen production.
- Postmenopause: Includes all the years after menopause. Effective treatment is crucial as many women spend a third of their lives in this stage.
During these stages, the ovaries reduce the production of estrogen, progesterone, and some testosterone. This hormonal decline triggers uncomfortable symptoms. HRT steps in to replace these missing hormones, alleviating symptoms and restoring well-being.
For more detailed information about how this therapy works, you can explore more info about Hormone Replacement Therapy.
The Main Symptoms HRT Can Treat
Menopausal symptoms can be life-disrupting, but hormones and HRT can provide significant relief. Key symptoms include:
- Vasomotor Symptoms: This category includes hot flashes (sudden, intense feelings of heat) and night sweats (hot flashes during sleep), which disrupt daily life and rest.
- Genitourinary Syndrome of Menopause (GSM): This refers to changes in the vaginal and urinary tracts. Vaginal atrophy (thinning tissues) leads to dryness and painful intercourse, affecting intimacy and comfort.
- Mood Swings: Hormonal shifts can cause irritability, anxiety, and feelings of sadness.
- Sleep Disturbances: Beyond night sweats, hormonal changes can make it difficult to fall or stay asleep.
- Brain Fog: Many women experience frustrating memory lapses and difficulty concentrating.
- Reduced Libido: A combination of physical discomfort and hormonal changes can lower sexual desire.
HRT offers a path back to feeling more like yourself by addressing these symptoms directly.
The Hormones Involved in Therapy
Understanding the key hormones in HRT helps in making informed decisions:
- Estrogen: The primary hormone that declines during menopause. It regulates the reproductive system, maintains bone density, and keeps vaginal tissues healthy. Its decline has widespread effects.
- Progesterone: Crucial for women with a uterus. Progesterone (or its synthetic form, progestin) provides endometrial protection by preventing the uterine lining from thickening when taking estrogen, which reduces cancer risk.
- Testosterone: This hormone also declines with age. While not FDA-approved for female menopause symptoms, some women benefit from small amounts for energy, mood, and libido, prescribed by experienced providers.
The combination of hormones used in HRT is highly individualized based on your symptoms, medical history, and whether you've had a hysterectomy.
For more comprehensive information about how these hormones work specifically for women, check out Hormone Therapy for Women.
The Comprehensive Guide to Hormones and HRT Treatments
Finding the right hormones and HRT treatment requires individualized medical consultation. Every woman's body is different, and the best approach is one custom to your specific needs.

| Type of HRT | Targeted Symptoms | Forms | Systemic Absorption |
|---|---|---|---|
| Systemic HRT | Hot flashes, night sweats, mood swings, bone loss, widespread menopausal symptoms | Oral pills, skin patches, gels, sprays, subcutaneous pellets | Absorbed into the bloodstream, affects the entire body |
| Local HRT | Vaginal dryness, painful intercourse, urinary symptoms (Genitourinary Syndrome of Menopause) | Vaginal creams, tablets, rings | Primarily affects the local tissue, minimal systemic absorption |
Understanding the different types of hormones and HRT
HRT can be a full-body approach or provide targeted relief.
- Systemic HRT delivers hormones throughout the body via the bloodstream. It's ideal for widespread symptoms like hot flashes, night sweats, mood swings, and bone loss.
- Local HRT delivers low-dose estrogen directly to vaginal tissue via creams, tablets, or rings. It's a great option for women who only need relief from vaginal dryness and urinary symptoms, as it has minimal systemic absorption and fewer risks.
Your medical history determines the specific type of therapy:
- Estrogen-only therapy is for women who have had a hysterectomy (uterus removal). Without a uterus, progesterone is not needed.
- Combined Estrogen-Progestin Therapy (EPT) is for women who still have their uterus. The progestin provides uterus protection by preventing the uterine lining from overgrowth, which reduces cancer risk.
How HRT is Administered
Modern hormones and HRT come in various delivery methods to fit your lifestyle:
- Oral pills: Convenient daily pills, but they are processed by the liver, which may slightly increase blood clot risk.
- Transdermal patches: Applied to the skin once or twice a week. They bypass the liver, carrying a lower blood clot risk than oral pills.
- Gels and sprays: Applied daily to the skin, also bypassing the liver.
- Vaginal rings, creams, and tablets: Provide targeted, local relief for vaginal symptoms with minimal whole-body effects. Rings are replaced every three months, while creams and tablets are used a few times per week.
- Subcutaneous Hormone Pellets: Tiny implants placed under the skin that provide steady hormone levels for several months, offering maximum convenience.
Common HRT Treatment Routines
Your treatment routine depends on your menopausal stage:
- Sequential HRT (or cyclical therapy) is for women in perimenopause. It involves daily estrogen with progestogen for 10-14 days a month, which mimics a natural cycle and causes a predictable monthly bleed.
- Continuous combined HRT is for postmenopausal women (no period for at least a year). It involves taking both estrogen and progestogen daily, which usually stops vaginal bleeding after an adjustment period.
The right routine for you will be determined in consultation with your provider based on your health and preferences.
Weighing the Evidence: The Benefits and Risks of HRT
The conversation around hormones and HRT has been confusing, largely due to initial interpretations of the Women's Health Initiative (WHI) trial from the 1990s. Initial WHI results suggested increased risks of breast cancer, heart disease, and stroke, which scared many women away from HRT.
However, further analysis revealed the "timing hypothesis": the risks were higher for older women (average age 63) who started HRT more than 10 years after menopause. When you start HRT matters. Today, we know that for healthy women starting HRT before age 60 or within 10 years of menopause, the benefits usually outweigh the risks. The duration of use also plays a role, making individualized assessment crucial. For the most current medical consensus, you can review The 2022 Hormone Therapy Position Statement of The North American Menopause Society.
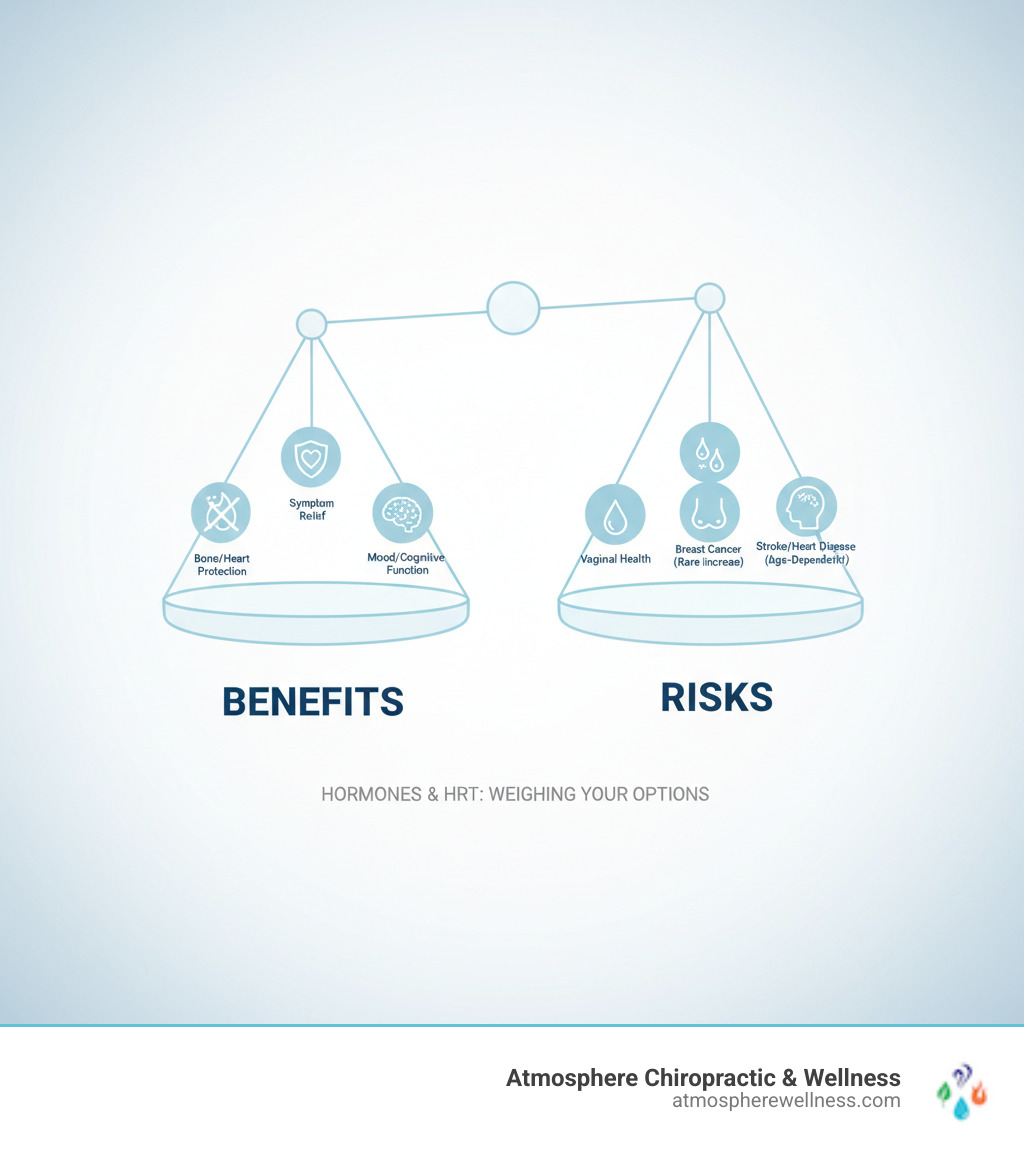
The Potential Benefits of Taking HRT
When used appropriately, the benefits of hormones and HRT can be life-changing:
- Symptom Relief: HRT effectively treats hot flashes, night sweats, and vaginal dryness, dramatically improving daily comfort and sleep.
- Bone Health: HRT is FDA-approved to prevent osteoporosis by slowing bone loss that accelerates after menopause, significantly reducing fracture risk.
- Mood and Cognitive Function: Many women report improved mental clarity, mood stability, and reduced "brain fog" with HRT.
- Cardiovascular Health: For women starting HRT before age 60, it may reduce heart disease risk by positively affecting cholesterol and blood vessels.
- Other Benefits: Some studies suggest a reduced risk of colorectal cancer. HRT also helps maintain skin moisture and elasticity.
Potential Risks and Side Effects
It's important to discuss potential risks, which are generally small for healthy women who start HRT at the right time.
- Blood Clots: Oral estrogen carries a small increased risk. Transdermal forms (patches, gels) largely avoid this risk as they bypass the liver.
- Stroke: Risk is slightly increased, particularly with oral HRT in older women.
- Heart Disease: Risk may increase if HRT is started more than 10 years after menopause, but may decrease for those who start earlier.
- Breast Cancer: Long-term use (5 or more years) of combined HRT (estrogen plus progestin) may slightly increase risk. Estrogen-only HRT has shown a neutral or slightly reduced risk.
- Ovarian and Uterine Cancer: Long-term combined HRT may slightly increase ovarian cancer risk. Uterine cancer risk increases if estrogen is taken without progestin in women with a uterus.
- Gallbladder Disease: Risk may increase, especially with oral estrogen.
Common side effects like breast tenderness, bloating, or headaches are usually mild and temporary, often resolving as the body adjusts. If side effects are bothersome, your treatment can often be adjusted. For more details, explore Bioidentical Hormone Replacement Therapy Pellets Side Effects.
Making an Informed Decision: Candidacy, Alternatives, and Modern Perspectives
Deciding on hormones and HRT is a process of shared decision-making between you and your provider. It involves a thorough risk assessment and a review of your symptoms, health history, and personal preferences to create the best plan for you.
At Atmosphere Chiropractic & Wellness, we partner with you to ensure you feel confident about your choices.
Who is a Good Candidate for HRT (and Who Should Avoid It)?
Many women are excellent candidates for HRT. Good candidates typically are:
- Healthy women under 60 (or within 10 years of menopause) with moderate to severe symptoms.
- Women needing osteoporosis prevention.
- Women with Premature Ovarian Insufficiency (POI), for whom HRT is essential for long-term health.
However, HRT is generally avoided by those with a personal history of:
- Hormone-sensitive cancers (e.g., breast, uterine).
- Blood clots, stroke, or heart attack.
- Unexplained vaginal bleeding.
- Active liver disease.
These are general guidelines; your individual situation requires a personal consultation.
Are Bioidentical Hormones a Safer Option?
Bioidentical hormones are chemically identical to human hormones, often derived from plants. It's important to distinguish between two types:
- FDA-approved bioidentical hormones (e.g., micronized progesterone, estradiol) are proven safe and effective through rigorous testing.
- Compounded bioidentical hormones are custom-mixed by pharmacies but are not FDA-regulated, meaning their long-term safety and efficacy are not well-established. The ACOG clinical consensus on compounded bioidentical hormones advises caution.
Our approach focuses on scientifically-backed treatments that are safe and effective.
The role of lifestyle factors with hormones and HRT
Hormones and HRT work best as part of a holistic wellness plan. Key lifestyle factors include:
- Diet: A whole-foods diet supports hormone processing and can reduce symptom severity.
- Exercise: Regular cardio and strength training improves mood, sleep, bone health, and can reduce hot flashes.
- Weight Management: Maintaining a healthy weight can lessen symptom severity.
- Stress Reduction: Managing stress through yoga, meditation, or other practices is crucial for hormonal balance.
- Smoking and Alcohol: Quitting smoking and limiting alcohol is vital, as both worsen symptoms and increase HRT-related risks.
Supportive Approaches to Hormonal Wellness
At Atmosphere Chiropractic & Wellness, we believe true wellness comes from an integrated approach. We combine hormones and HRT with complementary therapies to support your body's natural healing.
- Chiropractic Care: Proper spinal alignment supports the nervous system, which can positively influence your endocrine (hormone) system.
- Cryotherapy: Reduces inflammation, boosts mood, and improves sleep and energy.
- Red Light Therapy: Stimulates cellular repair to reduce inflammation, improve skin health, and boost vitality.
- Massage Therapy: Reduces stress, improves sleep, and relieves muscle tension.
Having these therapies under one roof in Lehi, Utah, allows for a unique, comprehensive approach. Combining HRT with these supportive treatments creates a synergistic effect for the best possible outcome.
Frequently Asked Questions about Hormones and HRT
Here are answers to some of the most common questions we hear from patients considering hormones and HRT.
How long is HRT typically taken and when should it be stopped?
There is no mandatory "stop date" for HRT; treatment duration is individualized. The goal is to use it for the shortest effective duration needed for symptom relief. An ongoing conversation with your provider is key to re-evaluate your needs annually. When stopping, a gradual taper is often recommended to minimize the return of symptoms.
Can HRT cause weight gain?
Scientific evidence shows that HRT itself does not cause weight gain. Instead, the metabolic changes of menopause often lead to weight gain, particularly around the midsection. By balancing hormones, HRT can help manage weight. Initial side effects like mild bloating or water retention are usually temporary.
Can I take HRT if I have a history of cancer?
This is a complex question requiring a highly individualized answer in consultation with your oncologist.
- For breast cancer survivors (especially hormone-sensitive types), systemic HRT is generally not recommended. However, local vaginal estrogen for severe symptoms may be an option.
- Women with a history of uterine cancer are also generally advised against HRT.
- For a history of other cancers, HRT may be possible, but each case requires careful evaluation by your full medical team.
Any decision about HRT after a cancer diagnosis requires a detailed discussion between you, your oncologist, and your HRT provider. For more, see research on Managing menopause after cancer.
Conclusion
Navigating hormones and HRT is about reclaiming control over your health during a natural life transition. For most healthy women who start modern HRT before age 60 or within 10 years of menopause, the benefits often significantly outweigh the risks.
Your health journey is unique. The decision to use hormones and HRT is an ongoing partnership with your healthcare provider, custom to your specific needs. It's not a one-time decision, but an evolving conversation focused on your goals.
At Atmosphere Chiropractic & Wellness in Lehi, Utah, we believe in a multi-angled approach to wellness. We know that combining HRT with our other innovative therapies--chiropractic care, cryotherapy, red light therapy, and massage--creates a powerful synergistic effect. This comprehensive approach helps you build a foundation for long-term vitality, not just manage symptoms.
If you're ready to see how balanced hormones and HRT, supported by our integrated wellness services, can help you reclaim your energy and confidence, we're here to help. Start your personalized HRT journey with us to experience comprehensive care.





